Does Medicaid Cover CPT G2211? A Comprehensive 2024 Guide
Navigating the complexities of healthcare billing and insurance coverage can be daunting, especially when dealing with specific Current Procedural Terminology (CPT) codes. If you’re asking, “Does Medicaid cover CPT G2211?” you’re likely seeking clarity on whether you can receive reimbursement for a specific healthcare service. This comprehensive guide aims to provide a definitive answer, delving into the intricacies of Medicaid coverage for CPT G2211, exploring related services, and offering insights to help you understand your healthcare benefits. We’ll examine the code, how it’s used, and the likelihood of Medicaid coverage, ensuring you have the most up-to-date information to make informed decisions about your healthcare.
This article goes beyond a simple yes or no answer. We’ll explore the nuances of Medicaid policies across different states, discuss potential requirements for pre-authorization, and offer tips for appealing denied claims. By the end of this guide, you’ll have a thorough understanding of CPT G2211, its relevance to your healthcare needs, and the steps you can take to maximize your chances of coverage. Our expert analysis and user-friendly approach will empower you to navigate the healthcare system with confidence.
Understanding CPT G2211: The Prolonged Services Add-on Code
CPT code G2211, introduced in 2021, is officially defined as a “Prolonged service(s) with or without direct patient contact provided by a physician or other qualified health care professional on the date of service; total time for the prolonged service(s) is 15 minutes to 29 minutes beyond the typical service time of the primary procedure when performed at the highest level.” In simpler terms, G2211 is an add-on code used to bill for extra time spent with a patient during an evaluation and management (E/M) service. It acknowledges the increasing complexity of patient care and the additional time healthcare providers often need to address complex medical issues.
Unlike other prolonged service codes that were previously used, G2211 is specifically designed to capture the additional time spent on a patient’s care beyond the typical time associated with the primary E/M service. This is particularly relevant in situations where patients have multiple chronic conditions, require extensive medication management, or present with complex psychosocial issues. The code aims to more accurately reflect the resources and expertise required to provide high-quality care in these complex cases.
It’s crucial to understand that G2211 is an *add-on* code, meaning it can only be billed in conjunction with a primary E/M code. It cannot be billed as a standalone service. Furthermore, the prolonged service must extend beyond the typical time associated with the highest level of the primary E/M service. This distinction is essential for accurate billing and reimbursement. For instance, if the highest level of an office visit typically takes 45 minutes, G2211 can only be billed if the total visit time exceeds 45 minutes plus an additional 15-29 minutes.
Key Concepts & Advanced Principles
To truly grasp the significance of G2211, consider these key concepts:
- Prolonged Services: These are services that extend beyond the typical time allocated for a standard E/M visit.
- Add-on Code: G2211 cannot be billed alone; it must accompany a primary E/M code.
- Time Threshold: The prolonged service must exceed the typical time for the highest level of the primary E/M service by at least 15 minutes.
- Documentation: Thorough documentation is crucial to support the use of G2211. The medical record must clearly demonstrate the medical necessity of the prolonged service and the amount of time spent.
A useful analogy is thinking of a standard recipe versus a complex gourmet meal. A standard E/M visit is like a basic recipe – it follows a predictable pattern and takes a set amount of time. A prolonged service, requiring G2211, is like a gourmet meal that demands extra preparation, attention to detail, and specialized techniques, ultimately requiring more time and effort.
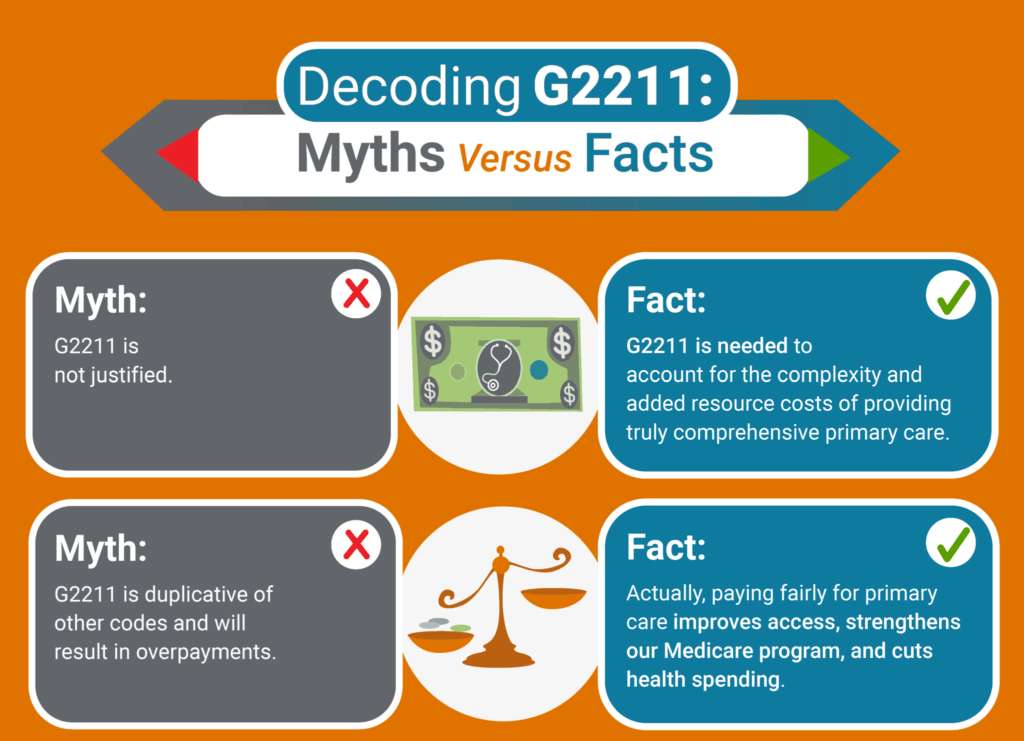
Importance & Current Relevance of G2211
CPT G2211 holds significant importance in today’s healthcare landscape due to several factors. Firstly, the increasing prevalence of chronic diseases and complex medical conditions necessitates more time and attention from healthcare providers. G2211 allows providers to be appropriately compensated for the extra time they spend managing these complex cases, ensuring they can continue to provide high-quality care.
Secondly, the code promotes accurate billing and transparency in healthcare. By specifically identifying and documenting prolonged services, G2211 helps to ensure that healthcare providers are reimbursed fairly for the resources they utilize. This, in turn, can help to improve the financial stability of healthcare practices and ensure that patients have access to the care they need.
Recent trends in healthcare, such as the shift towards value-based care and the increasing emphasis on patient-centered care, further underscore the importance of G2211. These models prioritize comprehensive, coordinated care that addresses the individual needs of each patient. G2211 supports these models by allowing providers to allocate the necessary time and resources to provide personalized care plans and address complex medical issues.
Medicaid Coverage Policies and CPT G2211
Now, let’s address the core question: Does Medicaid cover CPT G2211? The answer, unfortunately, isn’t a straightforward yes or no. Medicaid coverage policies vary significantly from state to state. While some states may readily cover G2211 when billed appropriately, others may have restrictions, limitations, or even explicitly exclude it from coverage.
The best way to determine whether your specific Medicaid plan covers CPT G2211 is to consult your state’s Medicaid website or contact your Medicaid provider directly. These resources can provide you with detailed information about covered services, billing requirements, and any necessary pre-authorization procedures. You can typically find contact information and policy manuals on your state’s Medicaid agency website. Search for your state’s Medicaid program online. For example, searching “Texas Medicaid” will lead you to the Texas Health and Human Services Commission website.
It’s also important to note that even if a state’s Medicaid program generally covers G2211, certain restrictions may apply. For example, some states may only cover G2211 when billed by specific types of providers, such as primary care physicians or specialists. Others may require pre-authorization for prolonged services exceeding a certain duration or frequency. Understanding these nuances is crucial for ensuring accurate billing and maximizing your chances of reimbursement.
Factors Influencing Medicaid Coverage
Several factors can influence whether Medicaid covers CPT G2211 in a particular case:
- State-Specific Policies: As mentioned earlier, Medicaid coverage policies vary significantly from state to state.
- Medical Necessity: Medicaid typically only covers services that are deemed medically necessary. The medical record must clearly document the medical necessity of the prolonged service and how it benefited the patient.
- Proper Documentation: Accurate and thorough documentation is essential for supporting the use of G2211. The documentation must include the start and stop times of the visit, a detailed description of the services provided, and the medical necessity of the prolonged service.
- Billing Requirements: Healthcare providers must adhere to specific billing requirements to receive reimbursement for G2211. This includes using the correct primary E/M code, ensuring that the prolonged service exceeds the minimum time threshold, and submitting the claim with the appropriate modifiers.
- Pre-Authorization: Some Medicaid plans may require pre-authorization for prolonged services, especially those exceeding a certain duration or frequency.
CareFirst BlueCross BlueShield and Prolonged Service Codes
CareFirst BlueCross BlueShield is a major health insurance provider in the Mid-Atlantic region. While not Medicaid, their policies can offer insights into how prolonged service codes like G2211 are handled by large insurers. CareFirst generally follows CMS (Centers for Medicare & Medicaid Services) guidelines, but it’s crucial to check their specific policy documents for the most accurate information. They may have specific requirements for documentation, pre-authorization, and eligible provider types.
Understanding how commercial insurers like CareFirst handle prolonged service codes can be helpful in anticipating potential challenges or requirements with Medicaid. While Medicaid operates under different regulations and funding structures, the underlying principles of medical necessity, proper documentation, and adherence to billing guidelines remain consistent.
Decoding CPT G2212: A Related Prolonged Service Code
While we’re focused on G2211, it’s important to briefly mention CPT G2212. This code is used for each additional 15 minutes of prolonged service beyond the initial 15-29 minutes captured by G2211. Think of G2211 as the initial “add-on” and G2212 as the subsequent “add-on” for even longer visits. Just like G2211, G2212 is an add-on code and requires proper documentation to support its use. Again, Medicaid coverage for G2212 will vary by state.
Strategies for Maximizing Medicaid Coverage for CPT G2211
If you believe you are entitled to Medicaid coverage for CPT G2211, here are some strategies to maximize your chances of approval:
- Verify Coverage: Before receiving services, contact your state’s Medicaid program or your Medicaid provider to confirm whether CPT G2211 is covered under your plan.
- Obtain Pre-Authorization: If required, obtain pre-authorization for prolonged services before the date of service. This will help to ensure that the service is covered and prevent potential claim denials.
- Ensure Proper Documentation: Work with your healthcare provider to ensure that the medical record accurately and thoroughly documents the medical necessity of the prolonged service and the amount of time spent.
- Appeal Denied Claims: If your claim for CPT G2211 is denied, don’t give up. You have the right to appeal the decision. Carefully review the denial notice and gather any additional information or documentation that may support your appeal.
- Seek Assistance: If you are struggling to navigate the Medicaid system or understand your coverage benefits, consider seeking assistance from a patient advocate or a legal aid organization. These resources can provide you with valuable guidance and support.
Real-World Value and Benefits of Proper Billing with CPT G2211
The proper use and coverage of CPT G2211 translates into tangible benefits for both patients and healthcare providers:
- Improved Patient Care: By allowing providers to allocate the necessary time and resources to address complex medical issues, G2211 can lead to improved patient outcomes and a better overall healthcare experience.
- Increased Access to Care: When providers are appropriately compensated for their time and expertise, they are more likely to be willing to accept Medicaid patients and provide comprehensive care.
- Financial Stability for Healthcare Practices: Accurate billing and reimbursement for prolonged services can help to ensure the financial stability of healthcare practices, allowing them to continue to provide high-quality care to their communities.
Reviewing the Landscape: CPT G2211 and Medicaid in 2024
As we move further into 2024, it’s essential to stay updated on the latest developments and policy changes related to CPT G2211 and Medicaid coverage. Keep an eye on announcements from CMS and your state’s Medicaid agency, as these organizations may issue new guidelines or clarifications that could impact coverage policies.
Insightful Q&A Section
- Q: What is the primary difference between CPT G2211 and other prolonged service codes?
A: CPT G2211 is specifically designed as an add-on code for prolonged evaluation and management (E/M) services, targeting the complexities that extend beyond the typical time for high-level E/M visits. Unlike some older codes, G2211 is intended to capture the additional time spent on patient care due to complexity, not just the duration of the visit.
- Q: If a Medicaid patient’s visit lasts exactly 15 minutes longer than the typical time for a Level 5 E/M service, can CPT G2211 be billed?
A: Generally, yes, CPT G2211 can be billed if the prolonged service is 15 minutes or more beyond the typical time. However, ensure the documentation clearly supports the medical necessity for the additional time.
- Q: What type of documentation is required to support billing CPT G2211 to Medicaid?
A: Comprehensive documentation is essential. This includes the start and stop times of the visit, a detailed description of the services provided, and a clear justification of the medical necessity for the prolonged service. It should explain why the extra time was needed and how it benefited the patient.
- Q: Can CPT G2211 be billed for telehealth visits under Medicaid?
A: This depends on the specific state’s Medicaid policy regarding telehealth. Some states may allow G2211 to be billed for telehealth visits if all other requirements are met, while others may have restrictions or exclusions.
- Q: What happens if Medicaid denies a claim for CPT G2211? What steps can be taken?
A: If a claim is denied, carefully review the denial notice to understand the reason for the denial. Gather any additional information or documentation that may support your appeal. You have the right to appeal the decision and should follow the appeals process outlined by your state’s Medicaid program.
- Q: Is pre-authorization always required for CPT G2211 under Medicaid?
A: Not always, but it’s prudent to check with the specific state’s Medicaid program or the managed care organization to confirm pre-authorization requirements. Some states may require pre-authorization for prolonged services, especially those exceeding a certain duration or frequency.
- Q: If a patient is seen by a physician and then spends an additional hour with a nurse, can CPT G2211 be billed?
A: CPT G2211 is typically billed by the physician or qualified healthcare professional who provides the prolonged service. Time spent with other staff members, such as nurses, may not be billable under this code unless the nurse also qualifies as a “qualified healthcare professional” under Medicaid guidelines and the prolonged service is within their scope of practice.
- Q: Are there any specific modifiers that should be used when billing CPT G2211 to Medicaid?
A: Yes, specific modifiers may be required depending on the state’s Medicaid program and the circumstances of the service. Consult your state’s Medicaid billing guidelines for the most up-to-date information on required modifiers.
- Q: How frequently can CPT G2211 be billed for the same patient within a given timeframe (e.g., monthly)?
A: There may be limitations on how frequently CPT G2211 can be billed for the same patient. These limitations vary by state and Medicaid plan. Review the state’s Medicaid policies to understand any frequency restrictions.
- Q: Does Medicaid coverage for CPT G2211 differ between fee-for-service and managed care plans?
A: Yes, coverage can differ. Managed care plans often have their own specific policies and requirements, which may be different from the state’s fee-for-service Medicaid program. Contact the managed care plan directly to confirm their coverage policies for CPT G2211.
Conclusion
In conclusion, determining whether Medicaid covers CPT G2211 requires careful investigation of state-specific policies and adherence to stringent documentation and billing requirements. While the code offers a valuable mechanism for recognizing and reimbursing healthcare providers for the extra time they spend managing complex cases, coverage is not guaranteed and varies considerably across different states. By understanding the nuances of Medicaid coverage for CPT G2211 and taking proactive steps to verify coverage, obtain pre-authorization, and ensure proper documentation, you can maximize your chances of receiving the healthcare benefits you are entitled to. Remember to consult with your healthcare provider and your state’s Medicaid program for personalized guidance and support.
The future of healthcare billing and reimbursement is likely to continue evolving, with an increasing emphasis on value-based care and patient-centered approaches. Staying informed about the latest developments and policy changes related to CPT G2211 and other healthcare codes is essential for both patients and healthcare providers. Share your experiences with navigating Medicaid coverage for CPT G2211 in the comments below. Your insights can help others better understand the complexities of the healthcare system and advocate for their healthcare needs.
